Transition of care for patients with End-Stage Renal Disease (ESRD) is a critical yet complex process, demanding meticulous attention to detail, especially when it comes to coding and billing. Accurate coding ensures proper reimbursement for services rendered and supports the financial viability of ESRD facilities. Understanding the evolving landscape of coding guidelines and payment adjustments is paramount for healthcare providers in this sector.
For facilities managing ESRD patients, staying abreast of programs like the Transitional Add-on Payment Adjustment for New and Innovative Equipment and Supplies (TPNIES) under the ESRD Prospective Payment System (PPS) is essential. While TPNIES primarily focuses on fostering the adoption of new technologies in dialysis care, its framework highlights the broader principles of reimbursement and coding accuracy within the ESRD landscape. This article delves into the key aspects of navigating transition of care for ESRD, with a focus on relevant coding guidelines and payment structures.
Effective transition of care in ESRD involves coordinating various services and ensuring seamless movement between different care settings, which could include hospitals, dialysis facilities, and home care environments. Each stage of transition necessitates precise coding to reflect the services provided, from initial assessments to ongoing management and the utilization of innovative equipment.
The Centers for Medicare & Medicaid Services (CMS) plays a crucial role in defining the coding and payment landscape for ESRD services. Programs like TPNIES, though specifically for new equipment and supplies, illustrate the agency’s approach to incentivizing advancements in ESRD care through targeted payment adjustments. To successfully navigate the financial aspects of ESRD care, particularly during transitions, providers must be familiar with the administrative and regulatory frameworks set forth by CMS.
For instance, the application process for TPNIES, now managed through the Medicare Electronic Application Request Information System (MEARISTM), underscores the importance of adhering to CMS guidelines. This system (https://mearis.cms.gov) is the gateway for ESRD facilities seeking to leverage payment adjustments for innovative technologies. The shift to MEARISTM for TPNIES applications, starting with CY 2025, emphasizes the increasing digitization and structured approach to healthcare administration within Medicare.
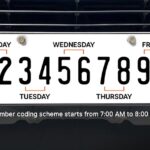
Alt text: Screenshot of the Medicare Electronic Application Request Information System (MEARISTM) portal login page, highlighting the entry point for ESRD facilities to submit TPNIES applications electronically.
The TPNIES program itself, as outlined in 42 CFR 413.236, is designed to ensure that ESRD beneficiaries have access to the latest renal dialysis equipment and supplies. By offering an add-on payment adjustment, CMS aims to mitigate the financial risks associated with adopting new technologies, thereby encouraging ESRD facilities to integrate innovative solutions into their care models. This, in turn, can significantly impact the quality and efficiency of transition of care processes.
Understanding the eligibility criteria for programs like TPNIES also sheds light on the broader principles guiding ESRD coding and payment. To qualify for TPNIES, equipment or supplies must meet several rigorous standards, including CMS designation as a renal dialysis service, novelty (application within 3 years of FDA approval), commercial availability, and innovation, as defined under 42 C.F.R. 412.87(b)(1). Furthermore, a complete Healthcare Common Procedure Coding System (HCPCS) Level II code application is mandatory, adhering to CMS coding guidelines.
These criteria emphasize the importance of accurate and timely coding submissions. For transition of care, this means that any new service or equipment utilized must be appropriately coded using the correct HCPCS Level II codes. Staying updated on the biannual coding cycles and deadlines, as detailed on the CMS website, is crucial for ESRD facilities to ensure compliance and optimize reimbursement.
The timeline for TPNIES determination and payment also offers insights into the broader administrative processes affecting ESRD facilities. CMS announces decisions on TPNIES applications as part of the annual ESRD PPS rulemaking, published in the Federal Register. This process, which includes proposed and final rules, allows for public comment and ensures transparency in decision-making. For ESRD facilities, this timeline underscores the need for proactive planning and timely submission of all required documentation to CMS.
Alt text: Image of the Federal Register seal and logo, representing the official journal of the federal government where CMS announces ESRD PPS rulemaking and TPNIES decisions.
Once a new equipment or supply is approved for TPNIES, CMS issues change requests with specific billing guidance. These change requests are crucial for ESRD facilities as they provide the technical instructions on how to report the new equipment or supply on ESRD PPS claims. The TPNIES period typically lasts for two calendar years, starting from January 1st, highlighting the temporary nature of this add-on payment and the need for facilities to adapt their financial planning accordingly. Access to these change requests is available on the CMS Transmittal page, a vital resource for staying informed about coding and billing updates.
In conclusion, navigating transition of care for ESRD patients effectively requires a comprehensive understanding of coding guidelines and payment adjustments. While programs like TPNIES are specifically focused on new and innovative equipment, they exemplify the broader principles of accurate coding, compliance with CMS regulations, and the importance of staying informed about evolving payment structures within the ESRD landscape. For ESRD facilities, mastering these aspects is not just about financial viability but also about ensuring that patients receive the best possible care during critical transition periods through the adoption of beneficial technologies and well-coordinated services.