Medicare’s Annual Wellness Visit (AWV) is a cornerstone of preventive healthcare, designed to proactively identify and address potential health risks. For healthcare providers, understanding the coding and billing nuances associated with AWVs is crucial for both financial health and quality patient care. While CPT codes like G0438 and G0439 are essential for service billing, the ICD-10 coding system simplifies preventive care coding, particularly when it comes to Medicare claims for these vital wellness visits.
Covered under Medicare Part B, AWVs are designed to be accessible, typically without co-pays for patients. These yearly assessments empower patients to collaboratively develop personalized care plans with their providers, ultimately leading to improved health outcomes. Reimbursement for AWVs is structured under Medicare’s Physician Fee Schedule, with rates varying based on the specific type of visit.
Navigating AWV Billing Codes: G0402, G0438, and G0439
The landscape of Medicare wellness visits includes different Current Procedural Terminology (CPT) billing codes, each reflecting a specific type of AWV. The timing and eligibility criteria are key differentiators in determining which AWV code is appropriate.
There are three distinct types of wellness visits:
- Initial Preventive Physical Examination (IPPE) (CPT code G0402): This “Welcome to Medicare” visit is a one-time preventive exam available within the first 12 months of Medicare enrollment.
- Initial Annual Wellness Visit (AWV) (CPT code G0438): This visit is for patients who have been enrolled in Medicare for over 11 months and may have missed their IPPE window. It serves as a comprehensive initial wellness assessment.
- Subsequent Annual Wellness Visit (AWV) (CPT code G0439): This is the yearly follow-up visit after an Initial Annual Wellness Visit, designed to review and adjust the patient’s personalized preventive care plan.
Let’s delve deeper into the descriptions of CPT codes G0438 and G0439, as they are central to ongoing preventive care.
CPT Code G0438: Initial Annual Wellness Visit
The Initial Annual Wellness Visit (G0438) mirrors the Initial Preventive Physical Examination in its comprehensiveness but is timed differently. It becomes available to patients after they have been enrolled in Medicare for 11 months or more. This is particularly relevant for individuals who did not utilize their one-time IPPE within the first year of Medicare enrollment. Importantly, even if a patient completed an IPPE, they are still eligible and should receive an Initial Annual Wellness Visit subsequently. This visit also incorporates an optional cognitive assessment and discussions around end-of-life care planning, adding to its preventive scope.
CPT Code G0439: Subsequent Annual Wellness Visit
The Subsequent Annual Wellness Visit (G0439) is the annual follow-up to the Initial Annual Wellness Visit. Patients become eligible for these visits eleven full months after their Initial AWV. These subsequent visits are crucial for proactively modifying and maintaining a patient’s preventive care plan, adapting to their evolving health status and needs at each given time.
Medicare Annual Wellness Visit Guidelines: A Focus on Prevention
Medicare’s wellness visit program is fundamentally a yearly health assessment, strategically designed to pinpoint health risks and collaboratively create a personalized care roadmap. It’s important to distinguish AWVs from traditional yearly physical examinations. AWVs offer a more holistic review of a patient’s medical history and lifestyle factors to formulate proactive care goals aimed at closing gaps in healthcare.
Wellness visits are especially beneficial for patients managing chronic conditions, providing a structured approach to care.
Through an AWV, a tailored care plan is developed to effectively manage existing chronic illnesses and schedule essential preventive screenings. This proactive approach enhances early disease detection and improves overall patient management.
Who Can Conduct AWVs?
While AWV billing must be under the direction of a provider with a National Provider Identifier (NPI) number, a significant portion of the assessment can be administered by clinical staff. This delegation of tasks optimizes physician time and involvement. Eligible providers who can direct AWV services include:
- Physicians
- Physician Assistants
- Nurse Practitioners
- Certified Nurse Midwives
- Clinical Nurse Specialists
- Pharmacists
Essential AWV Billing Requirements
To ensure accurate billing and claim approval, certain components are mandatory for inclusion in every patient’s wellness visit. These encompass:
- A comprehensive Health Risk Assessment (HRA)
- A thorough review and update of the patient’s medical and family history
- A detailed review of current healthcare providers, prescriptions/medications, and suppliers of durable medical equipment
- Measurement of vital signs including height, weight, blood pressure, Body Mass Index (BMI), and other routine measurements
- Provision of personalized health advice, targeted health education, and preventive counseling
- A clear list of identified risk factors, current medical and mental health conditions, and recommended treatment options
- A cognitive impairment screening to detect potential cognitive decline
- Development of a 5 to 10-year screening schedule for appropriate preventive services as recommended by Medicare guidelines
- An evaluation of the patient’s functional abilities and safety level, incorporating screenings for hearing impairments, fall risk, Activities of Daily Living (ADLs), and home safety assessment
- Identification of patients at risk for substance use disorders, including alcohol, tobacco, and opioid abuse
- Advance Care Planning discussions, addressing the patient’s wishes for future medical care
Submitting Clean Claims: ICD-10 and Annual Wellness Visits
Accurate claim submission is paramount for healthcare providers. When submitting a Medicare claim for an AWV, five key elements are required. This is where ICD-10 plays a crucial role in simplifying preventive care coding.
- A CPT Code that accurately reflects the specific type of AWV provided (G0402, G0438, or G0439).
- An ICD-10 code for a general adult medical examination (Z00.00). This code is specifically used for routine general medical examinations in the absence of any complaint, suspected or reported disease. Using Z00.00 is a key element of how ICD-10 simplifies the coding process for preventive services like AWVs, providing a standardized way to classify these encounters.
- Date of service – the date the AWV was performed.
- Place of service – specifying where the service was rendered (e.g., office, telehealth).
- Submit the provider’s NPI number for proper identification and billing.
Maintaining records of the care coordinator assigned to each patient can also be beneficial, particularly in the event of a claim audit.
Three Essential Steps for AWV Billing:
- Verify CMS Requirements: Ensure all Centers for Medicare & Medicaid Services (CMS) requirements for AWVs have been meticulously met and documented.
- Annual Claim Submission: Submit claims to CMS on an annual basis or at intervals that best suit your organization’s billing cycle.
- Check for Conflicting Codes: Confirm there are no conflicting billing codes that might lead to claim denials.
ThoroughCare: Streamlining AWVs and Closing Care Gaps
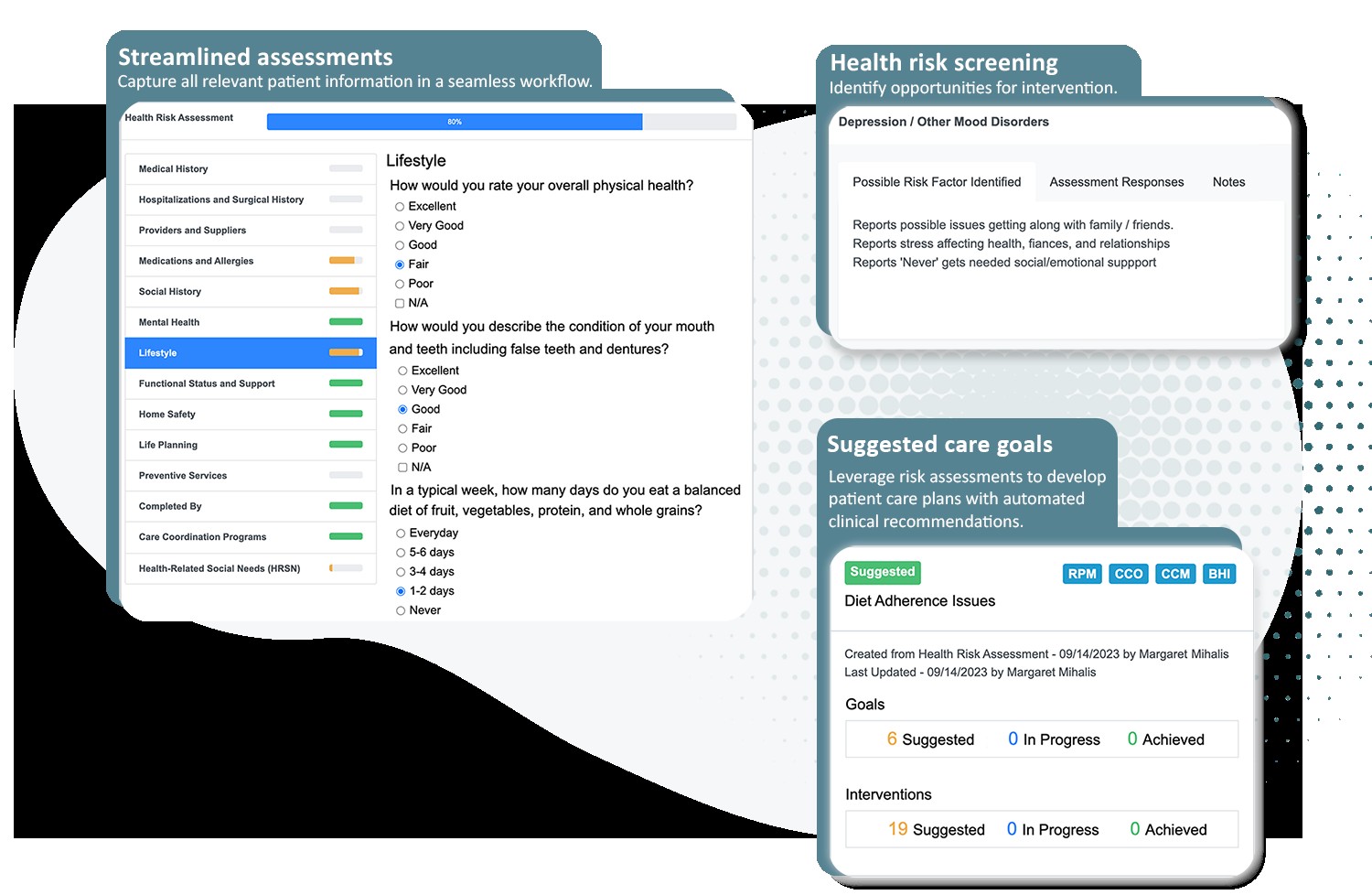
Alt text: Digital interface displaying an Annual Wellness Visit questionnaire, highlighting sections for Health Risk Assessment, Summary of Care, and design elements, emphasizing streamlined preventive care.
Value-Based Care and the Role of Annual Wellness Visits
AWVs are instrumental in promoting a value-based care model. By delving into a patient’s lifestyle, social history, mental health, and home environment, AWVs facilitate comprehensive patient risk stratification. This detailed understanding allows providers to develop personalized care plans that effectively address identified gaps in care.
This comprehensive approach enhances care coordination, streamlines collaborative decision-making, and strengthens the delivery of value-based care. AWVs have demonstrated effectiveness in fostering stronger provider-patient relationships, generating additional revenue streams, and contributing to overall healthcare cost savings.
Expanding AWV Services: Optional Add-ons
Medicare recognizes the value of comprehensive preventive care and supports additional CPT codes for optional services that can be seamlessly integrated with AWVs. These valuable add-on services include Advance Care Planning and Social Determinants of Health (SDOH) assessments.
Advance Care Planning: Empowering Patient Choice
Advance Care Planning is a crucial process that prepares patients for future medical decisions, particularly in situations of serious illness or when they may be unable to communicate their preferences. Advance Care Planning primarily revolves around two key documents:
- A living will, outlining treatment preferences
- A durable healthcare power of attorney, designating a decision-maker
During an AWV, providers can inquire whether patients have existing Advance Care Planning documents. If not, the AWV provides an opportune time to discuss these options and schedule dedicated sessions to complete a plan.
CPT Code 99497: Initial Advance Care Planning
CPT code 99497 is used for billing initial Advance Care Planning services, with an average reimbursement rate of approximately $79.57. To accurately bill for code 99497, the services must:
- Involve a face-to-face consultation lasting at least 30 minutes with the patient, and potentially family members or a surrogate (with a minimum of 16 minutes of documented service time).
- Be delivered by a physician or other qualified healthcare professional.
- Include a detailed explanation and review of advance care directives and the various options for completing them.
Documentation supporting at least 16 minutes of service time should clearly record the voluntary nature of the ACP conversation, summarize the topics discussed, identify all participants, and note the consultation duration. While completing an advance care directive during the ACP session is not mandatory for billing, it is fully covered for the patient when ACP is delivered in conjunction with an AWV.
CPT Code 99498: Additional Advance Care Planning
CPT code 99498 serves as an add-on billing code for extended Advance Care Planning services, accommodating consultations that exceed the initial 30 minutes. The average reimbursement rate for this code is around $68.90. Billing requirements include:
- Listing this claim separately, in addition to the primary consultation code (99497).
- Documenting a minimum of 16 minutes of service time beyond the initial 30 minutes, adhering to the same documentation guidelines as CPT code 99497.
Social Determinants of Health (SDOH) Assessment: Addressing Holistic Needs
Providers can effectively incorporate Social Determinants of Health (SDOH) data collection during AWVs. SDOH discussions, typically lasting between 5 and 15 minutes, should address crucial factors such as food and housing insecurity, transportation challenges, and utility difficulties.
The SDOH risk assessment is designed to identify factors that significantly influence the diagnosis and treatment of a patient’s medical conditions. While not solely a screening tool, it directly links to known or suspected SDOH needs.
CPT Code G0136: SDOH Assessment during AWV
Providers can receive additional reimbursement, approximately $18.44, for conducting SDOH assessments during an AWV by using CPT code G0136. This assessment is fully covered by Medicare when delivered as part of an AWV. To bill for CPT code G0136, providers must:
- Dedicate 5-15 minutes to SDOH discussion.
- Limit SDOH assessments to no more than once every 6 months per patient.
- Utilize a standardized, evidence-based SDOH risk assessment tool.
Medicare emphasizes the importance of following up on identified SDOH needs and actively connecting patients with relevant community resources.
Medicare AWVs in Federally Qualified Health Centers (FQHCs)
Federally Qualified Health Centers (FQHCs) are also eligible to bill for AWVs, but they utilize specific coding modifications to reflect their unique status.
In addition to the standard CPT codes for AWVs, FQHCs can use a special add-on code, G0468, to secure enhanced reimbursement.
For instance, if an FQHC provides an Initial Preventive Physical Examination, the clinic would bill using the combination of G0402 + G0468. This coding structure clearly indicates to Medicare that the service is being delivered through an FQHC. These organizations typically receive significantly higher average reimbursement rates compared to standard provider settings.
Leveraging AWVs for Care Management Enrollment
Annual Wellness Visits serve as an effective gateway for enrolling eligible patients in valuable care management programs and conducting supplementary assessments.
While some confusion may exist, AWVs can be billed concurrently with problem-oriented visits, provided they are not billed under the same code. Furthermore, several add-on services can be billed simultaneously with AWVs, including:
- Advance Care Planning (CPT codes 99497 and 99498)
- Depression screening (CPT code G0444) – Note: not permitted during the Initial AWV.
- Smoking cessation counseling (CPT codes 99406 and 99407)
- Obesity counseling (CPT code G0447)
- Substance use disorder screening and counseling (CPT codes G0442 and G0443)
CMS also permits clinicians to enroll patients in Medicare care management programs during the AWV if they meet eligibility criteria. The AWV provides an ideal opportunity to introduce patients to care management programs, highlighting the personalized health goals that align with the issues and risks identified during the wellness visit. Care management programs bring structure, consistency, and substance to the care plan, making it actionable and impactful.
Determining Appropriate Care Management Programs
The table below outlines general eligibility criteria for patient enrollment in various Medicare care management programs. This matrix can assist providers in identifying suitable programs for their patient populations and guide program offerings during AWVs.
Program Eligibility
To maximize the value of AWVs and boost enrollment in care management programs, establishing a clear workflow is essential. This workflow should outline patient engagement strategies before, during, and after the annual wellness visit.
ThoroughCare: Simplifying and Optimizing Annual Wellness Visits
ThoroughCare provides healthcare providers with the necessary tools and comprehensive support to enhance the effectiveness of their Annual Wellness Visit programs.
ThoroughCare assists providers in building new AWV programs or scaling existing services based on their specific organizational needs. ThoroughCare offers a robust software platform, clinical expertise to optimize workflows, and data and reporting assistance for continuous quality improvement.
ThoroughCare’s digital solutions include:
- An interactive Health Risk Assessment (HRA) tool
- Integrated screening tools such as ADL, CAGE, DAST-10, GAD-7, MDQ, PAC, PHQ-2, and a mini cognitive exam
- A consolidated care gaps summary with recommended interventions
- A comprehensive Personalized Prevention Plan Services report
- Robust care planning tools
- Automated CPT code assignment for accurate and efficient billing
*Reimbursement rates are based on national averages and may vary by geographic location. Always consult the Physician Fee Schedule on the CMS website for the most up-to-date information.